Project Charter
Part 1 |
||||||||
General Project Information |
||||||||
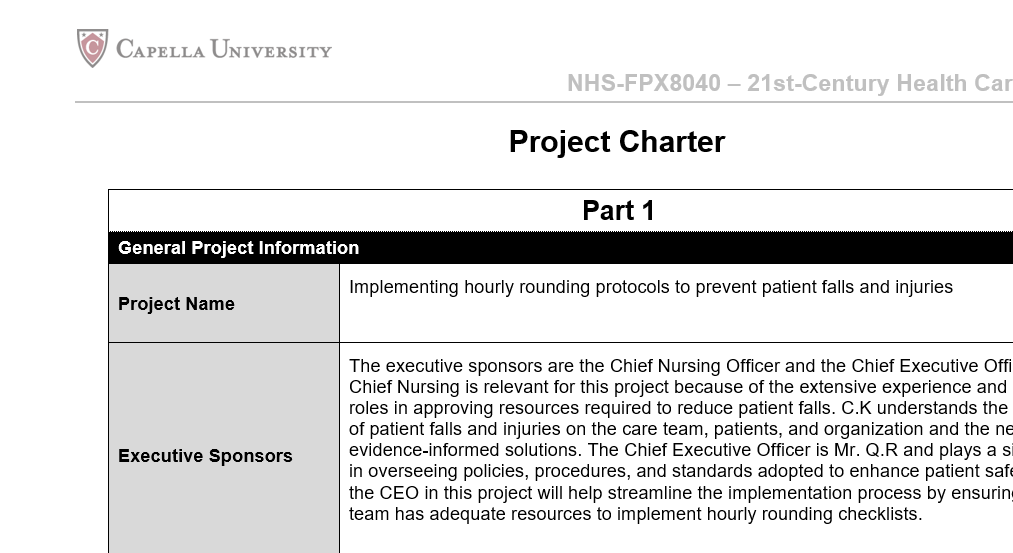
| Project Name | Implementing hourly rounding protocols to prevent patient falls and injuries
|
|||||||
| Executive Sponsors | The executive sponsors are the Chief Nursing Officer and the Chief Executive Officer. The Chief Nursing is relevant for this project because of the extensive experience and leadership roles in approving resources required to reduce patient falls. C.K understands the implications of patient falls and injuries on the care team, patients, and organization and the need for evidence-informed solutions. The Chief Executive Officer is Mr. Q.R and plays a significant role in overseeing policies, procedures, and standards adopted to enhance patient safety. Including the CEO in this project will help streamline the implementation process by ensuring that the team has adequate resources to implement hourly rounding checklists.
|
|||||||
| Department Sponsors | The departmental sponsor is V.S. The stakeholder is a nurse manager at the facility. He understands operational gaps and improvement opportunities available to increase the quality and safety of patient care. With over 10 years of working experience, the nurse manager is among the right contacts to initiate and sustain hourly rounding checklists and protocols to prevent falls and injuries. | |||||||
| Project Aim | The aim is to reduce patient falls and injuries in the acute care nursing unit. Hourly rounding checklists make the nursing team responsive to events in the clinical environment that could expose patients to falls and injuries. The intervention is appropriate for day and night shifts based on its structured nature and ability to promote patient-centered communication. In this case, the nursing staff, patients, and families interact to ensure the best outcomes. Adopting the hourly rounding checklist could enable White Plains to reduce patient falls by a significant margin within 10 weeks. In the end, patients and the facility benefit from reduced costs, shorter hospital stays, and reduced risk of readmissions. Thus, the organization can enhance its credibility by improving patient satisfaction. | |||||||
| Focus | The project focuses on adopting hourly rounding checklists to reduce patient falls and injuries. The tool allows the nursing team to proactively address sensitive patient needs, including increased vigilance to reduce the risk of nonfatal injuries and trauma-related incidences across the clinical setting. Hourly rounding checklists facilitate the accurate and complete assessment of environmental risks and hazards including the effectiveness of toileting assistance to reduce falls in patients admitted to critical care settings. As such, the nurse leaders will initiate an interdisciplinary process to enable everyone to understand the relevance of hourly rounding checklists and their roles in offering the desired assistance at all times. The Plan-Do-Study-Act (PDSA) will guide the team to understand scenarios involving patient falls and injuries and the collective efforts required to maintain zero incidences in the future.
|
|||||||
|
Project Team |
||||||||
| Title | Department | Credentials | Role | |||||
| Project Manager | T.F, Project manager | Nursing | Doctoral student | T.F: Project Manager
Will be in charge of the scope and deliverables. The member seeks to make meaningful improvements toward reducing patient falls and injuries using the hourly rounding checklist. The oversight role will ensure that everything runs according to the intended plan to enhance interdisciplinary collaboration and effective use of hourly rounding checklists in the critical care unit.
|
||||
| Team Members | The Nurse Manager | Critical care unit | Doctor of Nursing Practice | S.R: Nurse Manager
· 5 years of experience working in a critical care unit. Understands events in the clinical environment including patient vulnerability to falls and injuries. · Oversight and supervisory functions in the unit allow S.R to make informed decisions on improvements for optimizing quality and safety outcomes. · As the nurse manager, S.R gets the opportunity to play a significant role in increasing the hospital’s credibility through the effective use of hourly rounding safety checklists.
|
||||
| Advanced care nurse | Nursing | Advanced Practice Nurse and Doctor of Nursing Practice | P.K: Nurse overseeing the handling of patients with advanced care needs.
· The nurse has worked at White Plains for 10 years. · Being part of an advanced care setting means that she understands the complexities that expose individuals to falls and injuries. · Quality and safety measures are priority areas addressed by the advanced care nurse. · P.K will benefit through improved communication, interdisciplinary collaboration, and coordinated efforts that reduce burnout, risk of declining morale, and adverse outcomes. |
|||||
| Nurse educator | Nursing | Doctorate in Nursing Administration | R.A: A Nurse Educator
· Responsible for training the nursing team on new practices for optimizing quality and safety outcomes. · Coordinates with nurse leaders, HR, and staff to initiate evidence-based training programs on human, administrative, and technical changes required to improve care outcomes. · R.A will make significant contributions toward streamlining the use of hourly rounding checklists to achieve the intended results. |
|||||
Stakeholders |
||||||||
| The Project Leader | · The leader oversees procedures associated with designing, testing, and implementing hourly rounding checklists.
· Understands long-term plans and viable interventions for making the organization responsive to patients’ demands. · The leader will benefit from being in charge of one of the most promising initiatives that help boost the brand’s credibility. |
|||||||
| The project team | · The team is responsible for adhering to the scope and deliverables meant to optimize quality and safety outcomes.
· Members will share experiences, knowledge, and skills that make them responsive to calls for the organization to record zero falls and injuries in the future. |
|||||||
| Patients | · Patients are the primary beneficiaries of the hourly rounding checklists.
· Providing honest feedback will enable the project team to make improvements and ensure that the hourly rounding checklists cover all areas of the critical care unit. · Patients will benefit from reduced hospital stays, costs, readmissions, and complications associated with falls and injuries. |
|||||||
Part 2 |
||||||||
| Project Overview | ||||||||
| Project Description | ||||||||
| Include concise descriptions of who, what, when, where, and how long. Include a budget estimate if applicable. Describe the problem, how it was diagnosed, and how its solution aligns with strategic priorities. Include a timeline and required resources for the project: staff time, administrative resources, activity sites, and so on.
|
||||||||
| Evidence to Support Need | ||||||||
| Provide empirical and contextual evidence to support the gap, need, or improvement. Consider primary and secondary data sources, regulatory requirements, clinical practice guidelines, and benchmarking data. Be sure to include proper citations and descriptions of the integrity and reliability of any data you provide.
|
||||||||
| Project Purpose/Business Case | ||||||||
| Describe the business or clinical need this project addresses. What will the change or improvement accomplish and how will it impact consumers, staff, and the health care system as a whole?
|
||||||||
| SMART Objectives (Specific, Measurable, Attainable, Relevant, Time-Sensitive) | ||||||||
| Provide a concise list of objectives using the SMART model.
|
||||||||
| Project Scope | ||||||||
| Specify clearly what the project will and will not address. Include all relevant people and processes; this is an opportunity to address alignment to strategic organizational goals. Be sure to include a brief discussion of the project’s limitations.
|
||||||||
| Project Deliverables and Milestones | ||||||||
| Describe specific deliverables for each project phase. For the development and planning stage, team member recruitment from each involved department might be a deliverable, for example. If using PDCA, interim milestones may correspond to the completion of different PDCA cycles. Indicate timeframes in terms of the number of days, weeks, or months. Identify those responsible for each deliverable.
|
||||||||
Part 3 |
||||||||
| SWOT Analysis | ||||||||
| Strengths | ||||||||
| Project strengths could include things such as executive support or financial resources.
|
||||||||
| Weaknesses | ||||||||
| Identify at least three potential obstacles to a successful project outcome.
|
||||||||
| Opportunities | ||||||||
| Note current opportunities to facilitate project success, such as leveraging existing EMP to implement a clinical decision support system.
|
||||||||
| Threats | ||||||||
| Identify and rank (low, medium, high) at least three current or future threats to the project’s success, such as increased competition or high staff turnover in the affected department or service line.
|
||||||||
| Risk Level (Low, Medium, High) | Risk | |||||||
| Communication Strategy | ||||||||
| Indicate how the project manager will communicate to sponsors, the project team, and stakeholders. Describe the means and frequency of communication, including meetings, processes, and tools such as charts, wikis, and dashboards.
|
||||||||
| Constraints | ||||||||
| List any limits to personnel, funding, scheduling, or other options, such as a predetermined budget, limited staff, or deadlines, ethical use of data, et cetera.
|
||||||||
| External Dependencies Analysis | ||||||||
| If the project’s success may depend on external relationships or resources such as personnel, funding, communication channels, or community resources, describe them here. If there are no external dependencies, describe internal support.
|
||||||||
| Project Outcome Success Measures | ||||||||
| Describe measures that will be used to determine project success.
|
||||||||
| Metric | Outcome Measure | Process Measure | ||||||
| What is being measured to determine project success | Answers specifically final outcome (“So what?”), such as [X] percent patient satisfaction rate increase | Measures supporting final outcome such as compliance, time motion, competency | ||||||
| Data Collection and Management Plan | ||||||||
| Describe in detail the data you will collect and analyze to determine project success, including how and when it will be collected per the project milestones described above. Identify those who will collect, analyze, and store the data and address the integrity of the process (will it be done by team members or staff). Explain the integrity of the data sources: will data be collected from the EMR, online survey, or an internally created tool? Describe your plan to handle missing data and where you will securely store the data.
|
||||||||
| Ethical Considerations |
| Create guidelines to assure the ethical stewardship of patient data that take into account PHI, HIPPA, human subject considerations, equitable care, and IRB oversight, discuss any potential for human rights violations. Note any vulnerable populations involved and plans for equitable subject treatment. Describe data security factors: how data will be accessed and stored, including team members who will have access to personal health data and how it will be safeguarded (such as “Only [X] people will access the EMR”).
|
References
***END OF DOCUMENT***